 Health & Physiology
Health & Physiology
Taking cardiac fibrosis down with engineered immune cells
In many types of heart disease, cardiac tissue exhibits excessive extracellular matrix deposition, and fibrosis. This increases the stiffness of the heart, limiting its pumping capacity. By administering specially designed immune cells, which remove the cells responsible for fibrosis, we are able to diminish the quantity of fibrosis greatly.
Heart disease, in its many forms, is one of the most prominent causes of death and suffering, especially in developed countries. One of the hallmarks of most heart diseases is fibrosis, characterized by excessive deposition of the extracellular matrix. Limited amounts of this matrix normally occupy the spaces between the muscle cells of the heart to provide essential structural scaffolding. In the setting of heart disease, the matrix deposition becomes excessive and impairs the healthy heart's activity.
A specialized cell, called a fibroblast, is responsible for the production and maintenance of this matrix. In the setting of stress caused by the disease, including high blood pressure, too much matrix is produced. The resulting fibrosis stiffens the heart, decreasing the pumping function, such that insufficiently oxygenated blood is pumped to the rest of the body. Unfortunately, no therapies are targeting cardiac fibrosis, despite the high prevalence around the world.
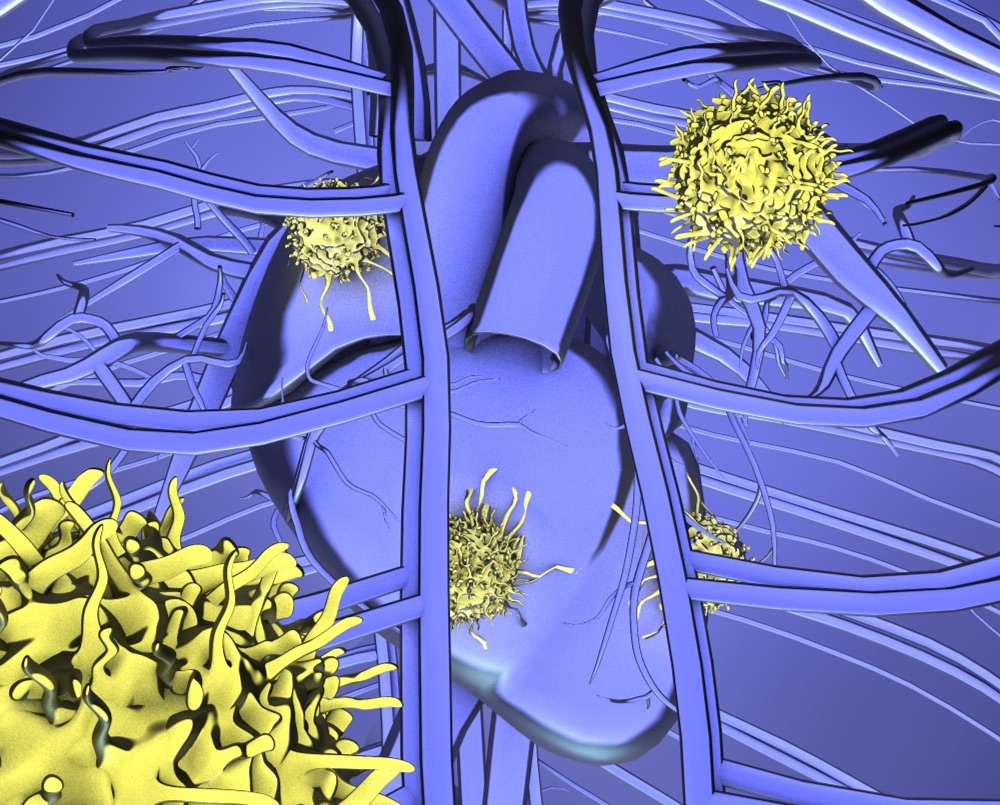
In the last two decades, cancer treatment has been transformed through the discovery and successful deployment of engineered immune cells as therapeutic drugs. T cells are a normal component of our immune system, which accurately identify and kill potential pathogens, such as bacteria. T cells use an antibody-like receptor on their surface to recognize a target cell that it can engage and destroy. In cancer therapy, T cells from the patient are engineered in the laboratory to produce a special recognition module called chimeric antigen receptor (CAR). Such a module allows the T cell to identify and kill the cancer cell. Thus, the patient's own immune cell is redirected to target and kill the cancer. The engineered T cells are called CAR-T cells.
We recently adapted this approach to use our own immune system to target and kill excessive cardiac fibroblasts in the setting of heart failure, thus extending the "immuno-revolution" beyond cancer.
To successfully develop this new CAR-T cell therapy, we first needed to identify a target (a protein) present only on the overactive fibroblasts. This unique protein is targeted by the engineered T cells so that they can recognize and kill the fibroblasts. Importantly, this protein must be absent in all healthy tissue, to avoid killing normal, healthy cells.
To identify potential targets, we inspected failing human hearts obtained from patients undergoing heart transplantation for severe heart failure, as well as healthy cardiac tissue for comparison. Through this approach, we could identify proteins present in failing, but not in normal hearts. One of the strongest candidates in failing hearts was a protein called Fibroblast Activation Protein (FAP). Fortunately, this protein does not appear to be present in healthy hearts or any other healthy adult organ.
With the identification of this potential target, we set out to test the ability of CAR-T cells to ablate unhealthy fibroblasts in mice with heart failure and abnormal fibrosis.
We used a well-established mouse model of heart failure produced by the administration of angiotensin II and phenylephrine, which mimic hypertensive heart disease caused by high blood pressure. In this progressive injury model, we observe prevalent fibrosis throughout the heart within seven days. At that point, we administered specialized CAR-T cells engineered to recognize and kill cells expressing FAP.
Three weeks after injecting FAP CAR-T cells, we observed a remarkable reduction in cardiac fibrosis compared to mice that received angiotensin II and phenylephrine but did not receive the engineered T cells. We also used ultrasound imaging (echocardiograms) and observed an improvement in heart function in the FAP CAR-T treated animals. The hearts of the CAR-T treated animals looked almost normal, while those without treatment had excessive fibrosis.
This proof-of-concept experiment is very exciting for two reasons. First, we demonstrate that CAR-T cell therapy may be applicable to prevalent health problems outside of oncology. Additionally, this experiment shows a marked reduction in fibrosis, a currently untreatable facet of heart failure. Even though our study was carried out in mice, we believe this approach could be useful in humans. CAR-T cells are already approved and in use for certain cancers, and our target was identified in failing human hearts. Before this type of therapy is ready for clinical use, a number of improvements must be made.
Our next step is to limit the length of time our CAR-T cells are active. Normally, CAR-T cells persist for decades in humans, which is desirable in cancer therapy for constant surveillance against tumor recurrence. However, fibroblasts are critical for tissue maintenance and healing after an injury. Therefore, we are looking into methods of inactivating the CAR-T cells after they perform their intended antifibrotic function. We are also developing methods of generating engineered T cells that only survive for a short time.
Another exciting direction of our research is to use these antifibrotic CAR-T cells in other diseases where fibrosis is also prevalent. Excessive fibrosis has been observed in many failing organs, including the kidneys, liver, skeletal muscles, lungs, and others. We intend to pursue similar animal-model studies to determine whether this therapy is more broadly applicable.
Our research offers a significant extension of T cell therapies beyond the field of oncology to impact one of the most common causes of human suffering and death: heart disease.
Original Article:
Aghajanian H, Kimura T, Rurik J et al. Targeting cardiac fibrosis with engineered T cells. Nature. 2019;573(7774):430-433.Next read: Chemotherapy and heart failure by Hector Villarraga , Mariana Garcia Arango
Edited by:
Massimo Caine , Founder and Director
We thought you might like
Empowering the immune system to fight against cancer
Oct 22, 2018 in Health & Physiology | 3.5 min read by Giovanni GermanoShuttle service for metastatic cancer cells
Aug 7, 2019 in Health & Physiology | 3 min read by Barbara M. Szczerba , Nicola AcetoMore from Health & Physiology
Tobacco smoking and other exposures shut off cancer-fighting genes
Aug 31, 2024 in Health & Physiology | 3 min read by Jüri Reimand , Nina AdlerA hidden clock that times cytoplasmic divisions
Aug 30, 2024 in Health & Physiology | 3 min read by Cindy OwWhen two kinases go for a dance
Aug 2, 2024 in Health & Physiology | 4 min read by Ioannis Galdadas , Francesco Luigi Gervasio , Pauline JuyouxAwakening the thymus to cure SARS-CoV-2 infection: a matter of genes
Jul 27, 2024 in Health & Physiology | 3.5 min read by Stefano Marullo , Cheynier RemiKeeping the balance: How epigenetics monitors cancer genes
May 13, 2024 in Health & Physiology | 4 min read by Zach Gray , Madison Honer , Johnathan WhetstineEditor's picks
Trending now
Popular topics


