 Neurobiology
Neurobiology
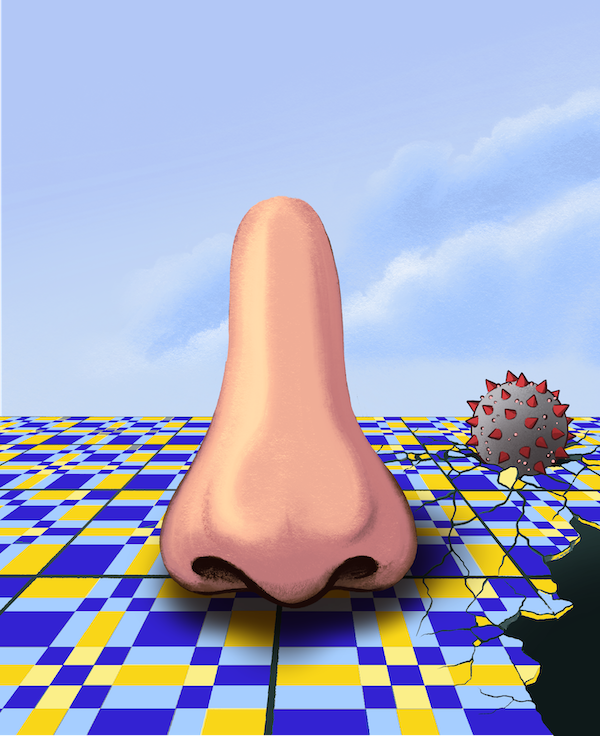
Solving the puzzle behind COVID-19 induced smell loss
The SARS-CoV-2 virus rarely infects olfactory sensory neurons yet causes widespread anosmia. To explain this apparent paradox, we found that odour detection is impaired due to virus-mediated disruption of nuclear architecture.
Smell is one of the fundamental senses in life: responsible for the recognition of environmental hazards, such as gas leaks, smoke inhalation, and spoiled foods, and yet also essential to our ability to enjoy meals beyond simple nourishment, appreciate the scents that define our environment, and evoke startlingly vivid memories. Olfactory perception has significant prognostic consequences, where loss is associated with the progression of neurodegenerative diseases such as Alzheimer's and Parkinson's.
COVID-19 pandemic elevated the smell loss, or anosmia, to a renewed focus, highlighting it as a hallmark symptom of infection with SARS-CoV-2. Unlike diminished odorant perception that often accompanies other viral upper respiratory infections, COVID-related anosmia appears without obvious nasal congestive symptoms. It quite often manifests as the only symptom for otherwise asymptomatic patients. For most, this condition lasts for a few weeks following viral infection. For other less fortunate individuals, olfactory dysfunction persists for months or, in some cases, years. Despite early investigative efforts, how SARS-CoV-2 inflicts sudden and occasionally persistent olfactory dysfunction has remained a mystery.
In our study, we approached the question using molecular evaluation of human olfactory epithelium from subjects succumbing to COVID-19 and a hamster model of SARS-CoV-2 infection, aiming to understand whether olfactory sensory neurons, the cells responsible for smell recognition, are the source of olfactory loss due to their direct infection. Using single-cell RNA-seq, a method akin to un-blending a smoothie, where each cell type in the mix can be identified, we revealed that SARS-CoV-2 enters the olfactory system via supporting or SUS cells. This approach only identified a negligible number of infected olfactory nerves. Nevertheless, although not directly infected, olfactory neurons appeared to stop the production of olfactory receptors. These receptors are proteins that recognize many odors, such as those giving coffee, chocolate, and roses their distinctive aroma. Together with olfactory receptors, key genes for the olfactory process were also affected - suggesting a cause for the absence of smell.
Our genome harbors almost a thousand olfactory receptor genes. About 5% of our genome is dedicated to odor recognition. Olfactory nerves follow a "one cell, one receptor" rule, and each neuron expresses only a single olfactory receptor gene while selectively ignoring others to facilitate accurate odor perception. This process requires a very sophisticated spatial organization of olfactory genes inside the 3D space of the cells' nuclei. To assess the integrity of this process in infected patients, we used techniques capable of revealing how genes within chromosomes talk to each other. In healthy cells, olfactory receptor genes are brought together into the same space, ensuring the normal receptor-manufacturing process remains in motion.
Surprisingly, the nuclear architecture in COVID-19 human specimens and SARS-CoV-2 infected hamsters is disrupted despite a direct infection that predominantly affects supporting sustentacular cells and not the actual olfactory neurons. As a result of dramatic damage of chromatin architecture, olfactory receptors and other olfaction-related molecules are downregulated and lack normal function. For COVID-19 patients, this molecular disturbance manifests as anosmia.
To figure out how a virus that doesn't infect olfactory nerves causes dramatic nuclear reorganization, we performed an experiment where serum (the portion of blood deprived of any cells) from an acutely infected hamster was applied to a naïve animal following UV irradiation to ensure the absence of any viral particles. This elegant approach revealed the damage of nuclear architecture as soon as 12.5 hours post serum inoculation, while mock infection showed regular genomic organization. Thus, we conclude it's not the virus per se but rather acute systemic changes caused by SARS-CoV-2 infection that alter the function of nerves that the virus cannot infect.
Our findings have important implications: i) adult neurons in the brain also rely on long-range and inter-chromosomal contacts between their neuronal gene families for proper function. We can infer from our study that dissipation in these contacts may contribute to long-lasting neurological effects observed in numerous patients. ii) olfactory receptor genes' expression may serve as a marker indicating maladaptive changes in the human body for a variety of conditions from viral infection to neurodegenerative diseases.
Original Article:
Zazhytska, M. et al. Non-cell-autonomous disruption of nuclear architecture as a potential cause of COVID-19-induced anosmia. Cell 185, 1052-1064.e12 (2022).Next read: When the girdle of social timing relaxes: Effects of the COVID-19 lockdown on human sleep by Christine Blume , Marlene H. Schmidt
Edited by:
Massimo Caine , Founder and Director
We thought you might like
Coronaviruses: Contagious Beasts and Where to Find Them
Apr 3, 2020 in Evolution & Behaviour | 4 min read by Anatoly KozlovThe Face Mask Dilemma: to wear or not to wear, that is the question
Apr 6, 2020 in Health & Physiology | 4 min read by Reinier ProseeThe evolution of the new coronavirus: what the past teaches us for a better future
Apr 9, 2020 in Evolution & Behaviour | 3.5 min read by Akira OhkuboThe life-span of SARS-CoV-2 in pediatric patients
Jun 9, 2020 in Health & Physiology | 3.5 min read by Sarah Gibson , Charlotte Zhang , Oulan Li , Yi XuMore from Neurobiology
Can we use a magnet to see brain inflammation?
Sep 25, 2023 in Neurobiology | 4 min read by Raquel Garcia-Hernandez , Santiago Canals , Silvia de SantisSurprising Behavior Changes in Genetically Modified Syrian Hamsters
Aug 30, 2023 in Neurobiology | 4 min read by Susan Lee , Kim Huhman , Jack TaylorTo achieve goals, we definitively need our neurons
Mar 10, 2023 in Neurobiology | 3.5 min read by Julien CourtinThe Impact of SARS-CoV-2 on the Brain: It Is All in Your Head
Feb 15, 2023 in Neurobiology | 3.5 min read by Meredith G. Mayer , Tracy FischerSolving A Decade-Long Mystery: Neurons Hold The Key To Rare Neurological Diseases
Feb 6, 2023 in Neurobiology | 3.5 min read by Anna-Leigh BrownEditor's picks
Trending now
Popular topics


